International Day of Immunology 2020: A spotlight on the Malaghan Institute
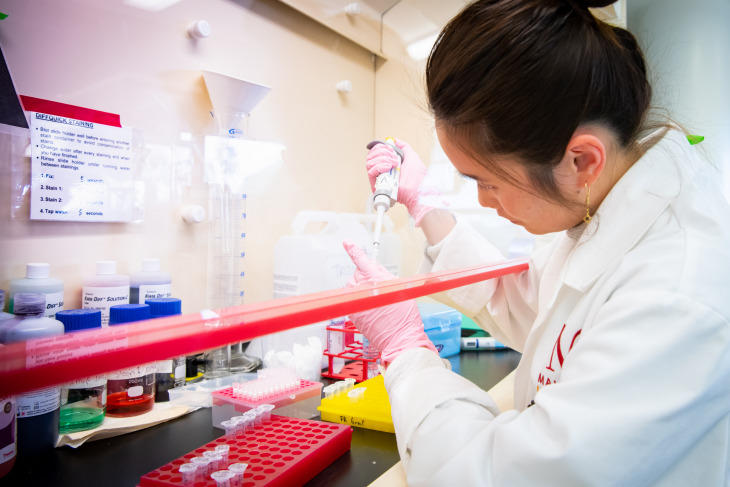
Immunology does not often whip the media into a frenzy. It doesn't always capture the public interest, and yet it is an integral part of so many biomedical disciplines. Today, on International Day of Immunology, we seek to highlight the importance and diversity of immunological research being supported by Cancer Research Trust NZ, and why it deserves to be front page news.
Celebrated each year on April 29, the day is dedicated to increasing global awareness of the importance of immunology in the fight against infection, autoimmunity and cancer. Here in New Zealand Kiwi researchers are undertaking innovative and varied research in the field of immunology. An example of this is the work of Dr Robert Weinkove and others at the Malaghan Institute of Medical Research, a world-leading independent biomedical research institute with a focus on breakthrough discoveries in immunology and immunotherapy. Since 2005, we have awarded the Institute funding for 10 Research Projects and 6 Professional Development awards.
“Big things can happen from small beginnings,” says Executive Director, Dr Douglas Ormrod. “We give bold ideas about cancer, including in the field of immunology, a chance to grow.”
Statistics show that almost everyone in New Zealand at some point will be affected by cancer in their lifetime, but with research identifying improvements and more effective treatment many people are living longer with cancer, and many cancers can now be cured.
“We fund research and professional development across the cancer spectrum from prevention, through detection, diagnosis and treatment to end of life palliative or hospice care. No other NZ cancer charity can claim this,” Dr Ormrod said.
Here's a look at some of the Kiwi-based research being undertaken at the Malaghan Institute of Medical Research that the Trust has funded: 
Anticancer drugs that target plasma membrane electron transport: evaluation in mouse models of cancer.
Dr Michael Berridge
$80,500
We have identified a new cancer drug target in the outer membrane of tumour cells and propose to investigate the effects of known drugs, and novel chemical compounds that interfere with this target, on the growth of tumours in mice. The approach being taken, which has not been previously attempted, will block cancer cell metabolism at the level of the cell membrane. This should eliminate the many undesirable side effects associated with most current anticancer drugs. In addition, multi-drug resistance should be avoided and preliminary results suggest that cancer cells may be sensitized to currently used drugs.
Phenotype and function of invariant natural killer T cells in chronic lymphocytic Leukaemia
Dr Robert Weinkove
$94,495
Chronic lymphocytic leukaemia (CLL) is the most common blood cancer in New Zealand Treatments are available, but presently CLL cannot be cured without bone marrow transplantation. The Malaghan Institute of Medical Research wants to harness patients' own immune systems in the fight against cancer. Working with Wellington Cancer Centre, the researchers will study the immune system of patients with CLL. They will analyse a rare blood cell called the invariant natural killer T cell and explore ways of stimulating patients' immune systems against their own leukaemia. This research will help the development of future cancer vaccination trials in New Zealand.
The trehalose dimycolates as potent immunomodulators in cancer therapy
Dr Bridget Stocker
$66,433
The immune system has a powerful role in the control of disease, yet often with cancer patients, the inherent immune response is not sufficient to control tumour growth. Macrophages are key immune cells that, on the one hand, are able to lead to tumour destruction, yet on the other hand, can also promote an increase in tumour burden. To convert the dysfunctional, tumour-promoting macrophages to ones that can be used to fight tumours, we are developing small molecules that will ‘switch' the macrophage to an activated state that will lead to tumour regression.
BCL6 and Chemoresistance: A new target for glioblastoma multiforme therapy?
Dr Melanie J. McConnell
$76,278
Glioblastoma multiforme (GBM) is the most common, and most aggressive brain tumour, and it has a very poor prognosis. GBM are highly resistant to radiation and chemotherapy, and turn on multiple survival pathways in response to chemotherapy. We will determine whether BCL6, a protein important for chemoresistance in lymphoma and leukemia, is expressed in the GBM cells that survive chemotherapy.
Targeting signalling pathways to refine the generation of anti-tumour T cells
Dr Shujie He
$85,345
Immune T cells isolated from tumour patients can be cultured ex vivo to large number, and transferred back to the same patient to induce tumour regression and improved survival. However, the ex vivo activation conditions can have huge effects on the therapeutic effectiveness of the transferred T cells. We will use current knowledge to optimize the activation conditions and examine the effects of critical factors that are known to regulate the production of functional T cells on tumour suppression. This information will guide the use of T cell activation strategies to improve cancer therapy.
Inhibiting Immune Checkpoints to Improve Immunotherapy for Brain Cancer
Dr Martin Hunn
$95,782
Cancer immunotherapies, which use a patient's own immune system to fight tumour cells, are now entering the clinic and have shown impressive efficacy against a number of cancers. One approach uses therapeutic vaccines, which work to educate the immune system and boost the number of tumour-destroying immune cells, while another is to remove the molecular brakes that constrain anti-tumour immune responses. We aim to test whether these two approaches can synergize to create a more effective cancer therapy, and propose to test this using our vaccine in a preclinical model of brain cancer.
NF-kB signalling in glioblastoma cells exposed to high-dose ascorbate and radiation
Dr Melanie McConnell
$89,691
People with glioblastoma multiforme (GBM) have a very poor prognosis because this cancer is extremely resistant to radiation therapy. Radiation causes DNA damage, but GBM tumours respond by ramping up their damage repair pathways, making them essentially resistant to radiation. We have shown that high-dose vitamin C makes GBM cells more sensitive to radiation by causing more DNA damage than radiation alone, while inhibiting DNA repair. We hypothesize that high-dose vitamin C inhibits activity of the survival factor NF-kB, and when combined with radiation will prevent NF-kB from repairing DNA.
Metabolic Constraints on Tumour Metastasis
Dr Mike Berridge
$83,676
Tumour metastasis is the main cause of mortality in cancer. Our novel finding that metastatic melanoma cells that have no mitochondrial genome, and whose energy metabolism is therefore purely glycolytic, fail to form tumours in the lung, raises the question of whether metabolic flexibility is essential for metastasis. We will investigate this phenomenon in metastatic melanoma and breast carcinoma cells. Manipulating mitochondrial metabolism is a potential therapeutic approach to metastatic cancer.
Boosting human anti-cancer immune responses using a glycolipid-conjugated vaccine
Dr Rob Weinkove
$110,533
Many cancers respond well to initial treatment, but subsequently relapse. Stimulating the immune system to destroy cancer cells may reduce this risk. However, patients' immune systems are often weakened by cancer itself or by chemotherapy. We have found a powerful way to activate immunity by stimulating unique types of ‘innate' white blood cell. Developed in collaboration with Callaghan Innovation, our new compounds combine conventional vaccines with this approach. Preliminary experiments show this may boost cancer-targeting immune cells. This project will investigate the effect of these compounds on human cells, with a view to developing a new class of cancer vaccine.
Sensitivity of ALL leukemic blasts to the isoflavene anticancer drug, phenoxodiol
Dr Patries Herst
$5,000
Phenoxodiol, currently in Stage III clinical trials for the treatment of late stage drug-resistant ovarian cancer and early stage prostate cancer, is generally well tolerated by patients. We have shown that phenoxodiol also kills lymphoid cancer cells. This project will test the effect of phenoxodiol alone and in combination with drugs currently used to treat acute lymphoblastic leukemia (ALL) on the survival of lymphoid blasts from bone marrows of patients with ALL. The results of this pilot study may contribute to the development of clinical trials involving phenoxodiol, and to improved treatment of childhood and adult ALL.
Combining immunotherapy with targeted drug therapy in melanoma: effects of the BRAFV600E-targeting drug, PLX4720, on antitumour immune responses
Dr Mike Berridge
$49,796
YB-1 is a protein found in breast tumours that promotes their growth and high levels are linked with poor outcomes New generation drugs that target tumour-specific proteins are showing promise in clinical trials. In advanced melanoma patients whose tumours carry the BRAFV600E mutation, vemurafenib generates dramatic early responses and prolongs survival by several months. Nevertheless, long-term prognosis remains poor. Combination therapies are needed that increase long-term survival and reduce dependence on costly drugs. Immunotherapy has the potential to be combined with highly-targeted drugs that should not be immunosuppressive. In this project we will determine whether the BRAFV600E-targeting drug, PLX4720, affects antitumour immune responses. This knowledge will pave the way for combining immunotherapy with targeted melanoma drugs in preclinical and clinical trials.
